Empower Your Skills, Boost Your Medical Coding Game! Lets start with Colonoscopy Coding.
Welcome to the fascinating world of colonoscopy coding! This episode aims to demystify this complex topic and equip you with practical tips to conquer it with confidence.
Understanding Colonoscopy:
Let’s begin with the basics. A colonoscopy, as you know, examines the colon and rectum for polyps, cancers, or other abnormalities. It uses a long, flexible tube equipped with a camera to visualize the entire colon.
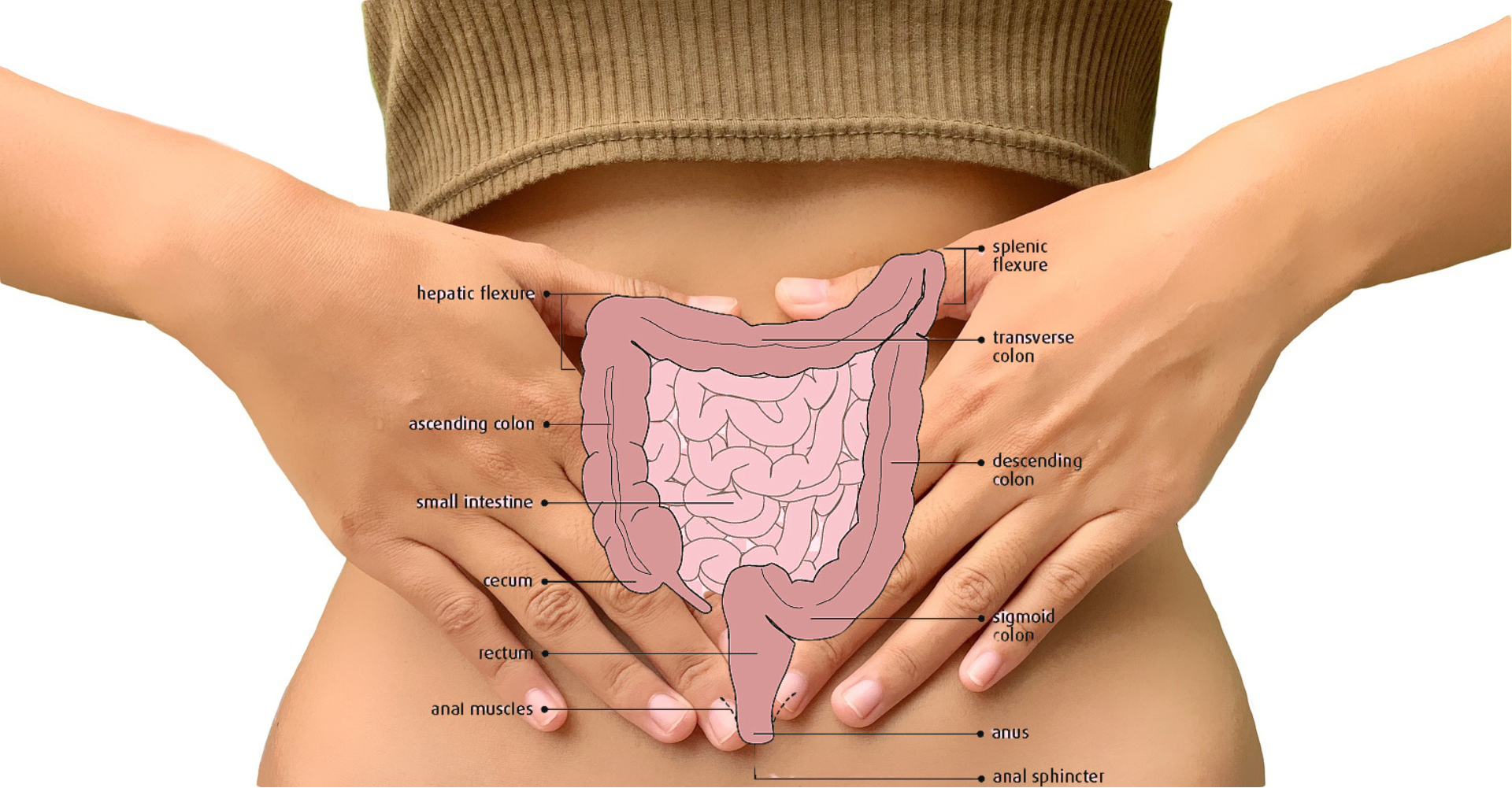
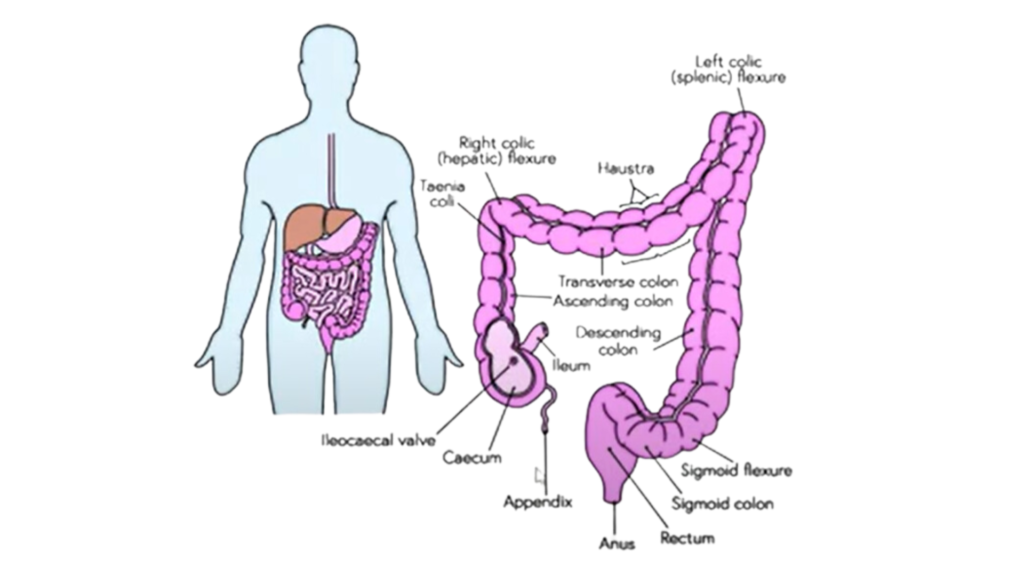
Before proceeding further lets understand the anatomy of colon and rectum.
The colon and rectum are the final parts of your digestive system, responsible for processing waste products and eliminating them from your body. Here’s a breakdown of their anatomy:
What is The Colon?
The colon absorbs water and electrolytes from waste material, forming stool. It also houses gut bacteria that aid in digestion and produce beneficial nutrients.
Structure: The colon is a long, muscular tube about 6 feet (1.8 meters) in length. It’s typically divided into five sections:
- Cecum: The pouch-like starting point of the colon, located in the lower right abdomen.
- Ascending colon: Travels up the right side of the abdomen.
- Transverse colon: Stretches across the upper abdomen.
- Descending colon: Moves down the left side of the abdomen.
- Sigmoid colon: The S-shaped section that connects the colon to the rectum.
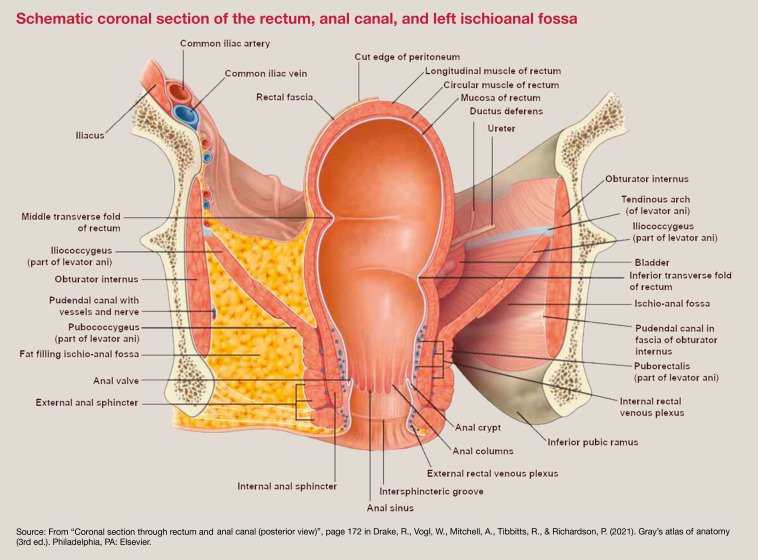
What is The Rectum?
The rectum serves as a temporary storage chamber for stool until it’s eliminated through the anus. It contains stretch receptors that trigger the urge to defecate.
Structure: The rectum is a short, muscular tube about 6-8 inches (15-20 cm) long, located in the lower pelvis.
Layers of the Colon and Rectum:
Both the colon and rectum share the same basic wall structure, consisting of four layers:
- Mucosa: The inner lining,containing cells that absorb water and electrolytes and produce mucus for lubrication.
- Submucosa: A layer of connective tissue containing blood vessels, nerves, and lymphatic vessels.
- Muscularis propria: A layer of smooth muscle that contracts to move stool through the colon and rectum.
- Serosa (outermost layer): A thin layer of tissue that covers the colon and attaches it to surrounding organs.
The colon and rectum are lined with millions of tiny hair-like structures called villi, which increase the surface area for absorption.
- The appendix is a small pouch attached to the cecum, but its function is not fully understood.
- Hemorrhoids are swollen veins in the rectum or anus, often caused by straining during bowel movements.
Types of Colonoscopies:
Four main types exist:
Screening Colonoscopy: Performed on asymptomatic individuals based on age, family history, and medical guidelines.
Diagnostic Colonoscopy: When the patient experiences symptoms like rectal bleeding or pain, requiring investigation.
Therapeutic Colonoscopy: Performed to remove polyps, tumors, or treat other abnormalities identified during diagnosis.
Surveillance Colonoscopy: For asymptomatic individuals with a history of polyps or colorectal cancer, requiring regular monitoring.
Coding Essentials:
Now, let’s crack the coding code!
The coding of a colonoscopy depends on several factors, including:
Reason for the procedure: Is it a screening colonoscopy for colorectal cancer, or is it being done to diagnose or treat a specific problem?
Procedures performed during the colonoscopy: Were any biopsies taken, polyps removed, or other interventions performed?
Patient’s insurance: Different insurance companies may have different coding requirements.
Screening Colonoscopy Coding:
CPT code:
Commercial and Medicaid Patients:
Use CPT Code 45378 (colonoscopy, flexible, proximal to splenic flexure; diagnostic) for both screening and diagnostic purposes. Remember, this applies to patients aged 50 and above.
Medicare Patients:
High Risk: Report HCPCS code G0105 (colorectal cancer screening; criteria for high risk as appropriate). High risk includes personal history of adenomatous polyps, colorectal cancer, inflammatory bowel disease, or specific family history.
Not High Risk: Use HCPCS code G0121 (screening for malignant neoplasm of colon).
ICD-10-CM Diagnosis:
When coding for screening, Z12.11 (Encounter for screening for malignant neoplasm of colon) should be your first-listed diagnosis.
Diagnostic colonoscopy Coding:
CPT code:
The specific code will depend on the procedures performed during the colonoscopy. Some common codes include:
45378: Colonoscopy, flexible; diagnostic, including collection of specimen(s) by brushing or washing, when performed.
45380: Colonoscopy, flexible; with biopsy, single or multiple.
45388: Colonoscopy, flexible; with ablation of tumor(s), polyp(s), or other lesion(s) (includes pre- and post dilation and snare or other excision).
ICD-10-CM Diagnosis:
The code for the specific condition being diagnosed, such as K57.1 (ulcerative colitis) or K63.8 (intestinal polyp).
Therapeutic colonoscopy Coding:
CPT code:
The specific code will depend on the procedures performed during the colonoscopy. Some common codes include:
45382: Colonoscopy, flexible; with control of bleeding, any method.
45384: Colonoscopy, flexible; with stent placement.
45386: Colonoscopy, flexible; with dilation, without snare or other excision.
ICD-10-CM code:
Use the code for the specific condition being treated, such as K61.8 (chronic intestinal obstruction) or Q39.2 (rectal prolapse).
Remember: This is just a general overview, and the specific coding for a colonoscopy will vary depending on the individual circumstances. If you are unsure about the correct coding for a particular procedure, it is always best to consult with a medical coder or billing specialist.
To learn more click to get the case study step by step.
Modifiers Made Easy:
Confused by the alphabet soup of modifiers? Don’t worry, I am going to guide you with the key players for colonoscopy coding.
Starring:
1-Modifier 33: The hero for preventive services! Use this when a routine colonoscopy turns into polyp removal or other interventions. It works for both commercial and Medicaid plans.
2-Modifier PT: Exclusive to Medicare, this modifier steps in when a screening shifts to diagnostic or therapeutic.
3-Modifier 52: When the colonoscope takes a detour before reaching the finish line (cecum), but still goes beyond the halfway point (sigmoid flexure), modifier 52 joins the party.
4-Modifier 53: If the colonoscope encounters technical woes or patient discomfort before reaching the final bend (splenic flexure), modifier 53 signals a mission abort.
Remember:
- Reviewing physician notes is crucial to understand the encounter and procedures.
- Stay updated on evolving guidelines and policies to avoid coding faux pas.
- Embrace coding manuals, online tools, and professional associations as your trusty sidekicks.
Bonus: This is just the first chapter! Future episodes will explore complex scenarios, polypectomy coding secrets, and masterclass tips for accurate and efficient coding.
So, ditch the modifier mayhem and conquer your colonoscopy coding with this handy guide!
Feel free to share your questions and doubts in the comments section below. Let’s conquer colonoscopy coding together!
Additional Resources:
American Medical Association (AMA): https://www.ama-assn.org/amaone/cpt-current-procedural-terminology
American Hospital Coding Association (AHIMA): https://www.ahima.org/
Centers for Medicare & Medicaid Services (CMS): https://www.cms.gov/
Remember, mastering medical coding takes time and practice. With dedication and these resources, you’ll be well on your way to coding colonoscopies like a pro!