
The process of billing claims and reimbursement is called “Revenue Cycle”. It’s not as simple as its definition. If the healthcare provider is new to private practice and insurance billing, the very first step in the revenue cycle is to get healthcare provider credentialed and obtain participating contracts with major payers of the service area.
What is credentialing and provider enrollment?
The process of “credentialing” and/or “provider enrollment” with an insurance network actually consists of two phases.
- Credentialing
- Contracting or Enrollment
The insurances ensure the eligibility of a healthcare provider according to their requirements for serving as in-network provider. For this purpose, they verify education, training and professional experience.
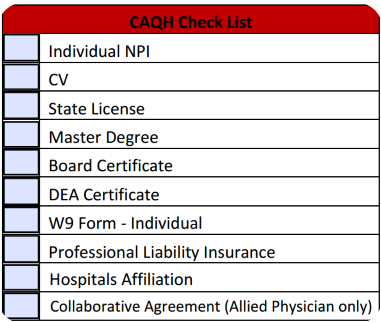
With a little planning this difficult task of getting doctor credentialed with payers can be made a bit easy. So, we prepare a checklist to make sure all the required information is presented before starting the process to avoid any delay.
We need to ask the healthcare provider:
- To establish a business entity under which to practice (LLC, S-Corp, C-Corp, etc) and get the tax ID
- For a sole proprietor, get a federal tax ID to operate under instead of SSN
- To get professional liability insurance policy
- To get an NPI number for provider individually (type 1) and for business entity (type 2)
- To be fully licensed in the state where he/she will provide services.
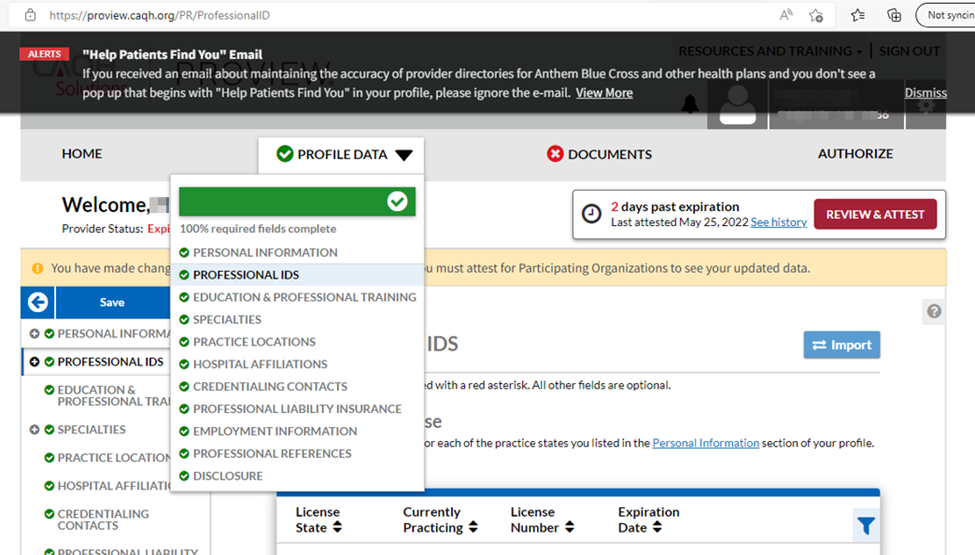
- To create a CAQH profile and keep it current.
- To have his/her practice location ready.
- To know which insurance networks, he/she want to participate with
CAQH check list example:
Contracting or Provider Enrollment:
After completion of required data submission & verification, now the phase is where insurance company issues a participating agreement. It defines the terms and conditions of participation, required to receive in-network reimbursements. This phase is called contracting or enrollment.
Note: Until the credentialing and enrollment process is completed, we can submit our claims to insurer for the doctor as out-of-network. But in this case, there is no guarantee whether the claims will be accepted, processed and reimbursed or not. It depends on the patient’s plan. Whether the plan’s policy has out of network benefits or not.
Moreover, Government Insurances, such as; Medicare and Medicaid won’t cover OON service.
Got Credentialed & Contracted. Now What??
Now, you’re ready to start billing the insurer network for the services on behalf of the healthcare provider. But there are some more tips to maintain the records.
- Access the insurance websites to confirm the provider is in their providers directory. Most of the insurance networks have access to eligibility & benefit verification, claims filing and follow-up, reimbursement information and other revenue cycle related activities on websites.
- Record all contact information for the insurance network related to credentialing, contracting and claim filing and follow-ups.
- Record your provider id, the effective date and estimated time for your next re-credentialing process.
- After a year of service, now it’s time to evaluate which insurance companies are providing patient volume
- Compare reimbursements to identify carriers to eliminate or renegotiate reimbursement rates
- Check and maintain your provider’s CAQH profile by quarterly attestations , re-attestations and document updates any time you renew an item such as license or malpractice/ liability insurance
For example:
- Keep your doctor’s NPPES records updated so that your NPI numbers always reflect accurate name, address, and other information
- Don’t neglect or ignore the re-credentialing requests from insurers or requests for renewed or additional documents. Because delayed or failed response can lead you to network termination.
Healthcare providers mostly trust companies such as Upfluencemd to outsource their practice startups and credentialing and enrollment process to ensure that their information is in safe hands.
For further training material on medical billing and coding, revenue cycle management and practice management, please visit my blog site health to insurance.



