The Merit-Based Incentive Payment System, or MIPS, is a program developed by the Centers for Medicare and Medicaid Services (CMS) that rewards healthcare providers for providing high-quality care to their patients. One of the key aspects of participating in MIPS is submitting data to the program. In this article, we will discuss how to submit data in MIPS and how it works.
Submitting Data in MIPS
The process of submitting data in MIPS involves several key steps: selecting measures to report, collecting data, submitting data, and receiving feedback on performance.
Selecting Measures to Report
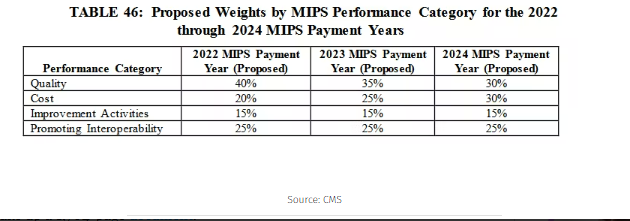
The first step in submitting data to MIPS is selecting the measures that you want to report on. There are several categories of measures that you can choose from, including quality, promoting interoperability, improvement activities, and cost.
Quality measures are designed to assess the quality of care that you provide to your patients. These measures are based on evidence-based guidelines and are designed to promote the best practices in healthcare.
Promoting interoperability measures are focused on the use of electronic health records (EHRs) and other health information technology (HIT) to improve care coordination and patient outcomes.
Improvement activities are focused on implementing specific activities that are designed to improve the quality of care that you provide to your patients.
Cost measures are focused on the cost of care that you provide to your patients. These measures are designed to encourage providers to provide high-quality care at a lower cost.
Collecting Data
Once you have selected the measures that you want to report on, the next step is to collect the data that you need to report on those measures. This may involve collecting data from your EHR, from patient surveys, or from other sources.
Submitting Data
Once you have collected the data that you need, the next step is to submit that data to MIPS. There are several ways to submit data to MIPS, including through a Qualified Registry, a Qualified Clinical Data Registry (QCDR), or directly through the CMS Web Interface.
Receiving Feedback on Performance
Once you have submitted your data to MIPS, you will receive feedback on your performance. This feedback will include information about how you performed on each of the measures that you reported on, as well as your overall MIPS score.
How MIPS Works
MIPS is a performance-based payment program that rewards healthcare providers for providing high-quality care to their patients. The program is based on a scoring system that takes into account several different factors, including quality of care, use of HIT, improvement activities, and cost.
Providers who participate in MIPS are eligible to receive a payment adjustment based on their score. The payment adjustment can be positive or negative, depending on how well the provider performs on the measures that they report on.
The MIPS program is designed to encourage healthcare providers to provide high-quality care to their patients, while also promoting the use of HIT and encouraging providers to implement specific activities that are designed to improve the quality of care that they provide.
In Conclusion
Submitting data in MIPS is an important aspect of participating in the program. By selecting the measures that you want to report on, collecting data, submitting data, and receiving feedback on performance, you can improve the quality of care that you provide to your patients, while also earning a payment adjustment based on your MIPS score.