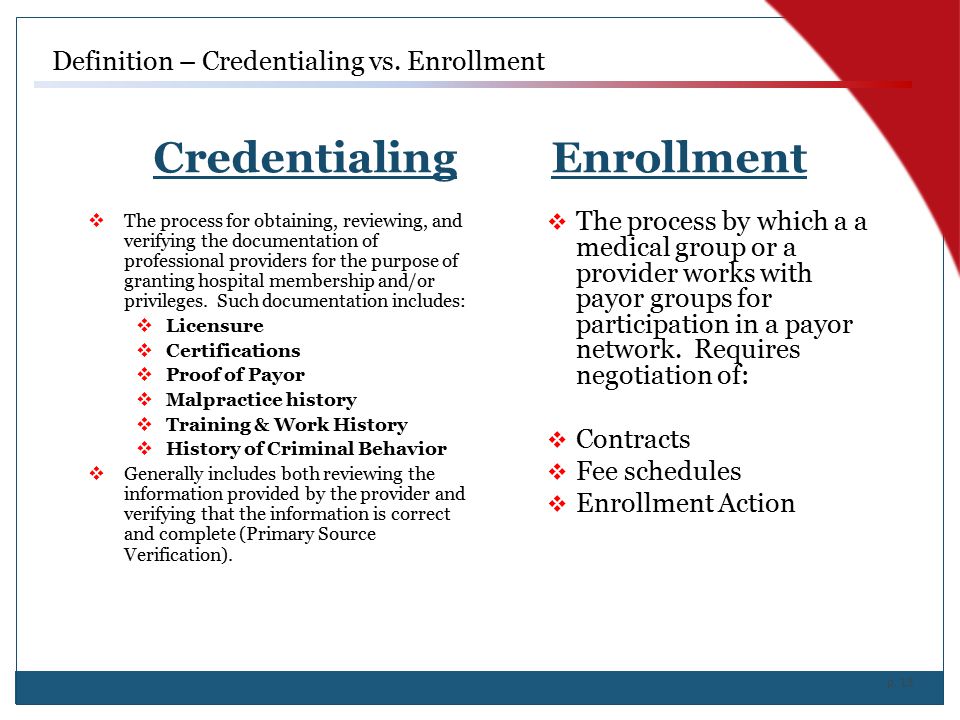
What’s the Difference between these two?
Credentialing Explained:
Validating a healthcare provider in a private health plan and the approval to join the network is credentialing
Enrollment Explained:
While enrollment represents to the process of requesting participation in a health insurance network as a provider. Payor Enrollment, Credentialing Bringing new healthcare providers on board is galvanizing, yet a complicated procedure with a lot of moving parts. If you’ve ever had the opportunity to work for a physician or mid-level professional at the start of a practice or you have hired one, you must know how much work is involved.
Importance of Payor Enrollment and Credentialing:
With the ever-shifting rules and regulation and legislature’s aspect, keeping up with the process of payer enrollment cannot be underestimated. It’s a chaotic and mind numbing process when you go for payer enrollment. But in spite of all the troubles its more essential, yet misunderstood piece of the puzzle.
One of the most vital concerns is to make your provider’s practice billable. It should sit atop of your to-do list. It can be done with proper know-how and information to avoid any sort of delays or rejections of the procedure. Because if you will be failed to stick to the mandatory timeline, however, can result in stoppage or delay in enrolling healthcare providers in to the health plans.
Procedural difference in Payer enrollment and credentialing?
Mostly, people are confused when it comes to payor enrollment vs. credentialing. Provider credentialing is the method by which we authenticate a healthcare provider i.e., a new physician’s qualifications – his/her credentials — eligibility to offer specified services and medical care.
This commonly takes in furnishing documentation of the person’s license, training, education, and career. It is, nevertheless, a chunk extra hard than it would sound, as, whilst possible, the facts originate from the source of the qualification, for instance, the medical school, licensing enterprise or agency and previous employer/practices.
In-network vs out-of-network:
On the other hand, payer enrollment is the procedure of registering healthcare providers with health plans. This is essential to make these providers “in-network” or “participating.” Being enrolled is necessary, as most patients simply won’t pay the higher copay to be seen out-of-network.
Why people don’t go for non-participating providers?? It costs them higher than to go to an in-network provider. Already, there is a steeply rising costs is making them pay for health coverage in the form of deductible and out of pocket expenses more 30 percent more than merely seven years ago.
If the question that, do you need to enroll in each and every payer US health insurance industry. Then the answer is “no”.
Process:
You only need to discover which health plans are most familiar in your area as a first step. Take a good look on various groups to determine which health insurers you want to do business with. Go for all major payors in the region.
First, you need to be certain whether your providers are enrolled with the top insurance companies or not, such as Aetna, United HealthCare, CIGNA, BlueCross/BlueShield, Humana, and, among others. In addition, there may well be a big number of regional payors that the patients who comes to you, might be using.
Of course, there is a must, which is the need to get enrolled with government-operated programs, such as Medicare and Medicaid. Keep in mind that these are a bit more complex, and all you need to give a plenty of time to complete the process within the set timeline.
Major Confusion About Payor Enrollment?
Where people underrate the amount of time, it takes to complete the enrollment process with each payor plan. It creates major issue that leads the practices to have issue in the process. There is a quantity of information involved in it so payers take time to evaluate and approve.
Time Legnth For Provider Enrollment:
Time length for the process may vary from one payor to the other payor and from one state to the other state. Holistically, it takes 30-90 days on average. But in some cases, there may be 4 to 6 months. Most insurances won’t allow you to start the procedure after the start date of provider.
Reasons to consider outsourcing the payor enrollment:
There are a lot of strong reasons why a growing number of healthcare providers is getting the services from outside firms to administer payor enrollment for their practices. Because getting professionals in this area brings a number of benefits.
Experience and Knowledge:
Companies, such as UpfluenceMD, not only have a comprehensive hold of payor enrollment and credentialing, but also the contacts, skills and awareness to make the process as easy as possible. Having a lot of experience, these companies also know how to magnify issues and appeal adverse decisions.
No enrollment errors:
Working experience of enrollment experts will significantly cut the possibility for enrollment data mistakes. It is the big cause of delays. This feature of making less errors will boost the total process and help you get your insurance payments as sooner as possible.
No employee training required:
You have to train the staff for the process and will have to place all the accountability on that one person. But if you outsource your payor enrollment, you would only be concerned about the end results. Your payor enrollment expert at UpfluenceMD will willingly remove all the troublesome tasks from your plate. He and/or she will send the necessary faxes and emails, perform the follow-ups and make the essential phone calls.

Why Should You Consider Outsourcing The Credentialing?
Speed, Quality and Cost Saving:
The main achievements of outsourcing your credentialing are speed, quality and cost savings. When there is a team all set with working experience of the process is more efficient to deliver the results. Then hiring, training and paying an in-house team is not a good idea. This gives your office staff to put the efforts on other chores related to your practice and your patients.
Medical provider credentialing is a basic task. The providers should be authorized by all payers to bill for services. The credentialing process should assure that the provider meets precise criteria set down by a health insurer. As a result, credentialing enhances patient’s trust, reduces the potential risks and gives a boost to the practice’s reputation.
Credentialing services such as UpfluenceMDcan often perform these services much quicker and without as many errors, which can also help you get more revenue and see patients faster.
There is another favor at getting credentialed by UpfluenceMD. They are offering credentialing and enrollment services FREE of cost if you buy their full revenue cycle management services. For detailed information on medical credentialing and payor enrollment, please contact the professionals at UpfluenceMD