How Revenue Cycle Management (RCM) Can Improve Healthcare Financial Performance
Revenue Cycle Management (RCM) is a financial process that enables healthcare organizations to track patient care services from the moment they are provided to the time they are paid. The RCM process includes patient registration, appointment scheduling, medical coding, billing, claims submission, and payment processing. By implementing an efficient RCM process, healthcare organizations can improve patient care, reduce costs, and enhance their financial performance. In this article, we will explore how data analytics, denials management, and payment posting can help to optimize the RCM process.
Improve Patient Care
One of the significant benefits of implementing an efficient RCM process is improved patient care. When healthcare organizations have an effective RCM system in place, it ensures that patients receive the right care at the right time. The RCM process starts with patient registration, where patient information is captured, and appointments are scheduled. This ensures that patients are seen by the appropriate healthcare provider without any delay. Once the patient has received care, the RCM process ensures that the correct medical codes are used to bill the insurance provider accurately. This helps to avoid any delays or denials in payment and ensures that the patient receives the appropriate care.
Reduce Costs
Another significant benefit of RCM is the reduction of costs. An efficient RCM process ensures that healthcare organizations are paid promptly for the services they provide. This reduces the risk of revenue loss due to claims denials, rejections, or delayed payments. It also ensures that healthcare organizations do not have to spend additional resources chasing down unpaid claims. By streamlining the billing process, RCM helps to reduce administrative costs, increase revenue, and improve cash flow.
Improve Financial Performance
RCM also plays a crucial role in improving the financial performance of healthcare organizations. By reducing administrative costs, increasing revenue, and improving cash flow, healthcare organizations can invest in new equipment, hire more staff, and expand their services. An efficient RCM process helps healthcare organizations to operate more effectively and efficiently, resulting in improved financial performance.
Full Revenue Cycle Management
Implementing an efficient RCM system can help healthcare organizations to improve their financial performance significantly. The healthcare RCM process involves various tasks, including patient registration, eligibility verification, coding, billing, claims submission, and payment processing. All these tasks must be completed accurately and in a timely manner to ensure that healthcare organizations are paid promptly and accurately for the services they provide.
Patient Demographics Registration:
Patient registration is the first step in the RCM process. This involves capturing patient information, insurance details, and appointment scheduling. An efficient patient registration process ensures that patients are seen by the appropriate healthcare provider without any delay. It also helps to reduce administrative costs by minimizing errors and rework.
Eligibility and Benefit Verification:
Most of the time we misinterpret both terms Eligibility and Benefit verification or E&B verification as a same thing but there is a difference between them. We need to understand that difference.
Eligibility Verification
Eligibility verification is another critical task in the RCM process. This involves verifying a patient’s insurance coverage and benefits. By verifying insurance coverage upfront, healthcare organizations can avoid claims denials and rejections, reduce administrative costs, and ensure that patients receive the appropriate care.
Benefits Verification
Insurance benefit verification is a crucial step in the RCM process. It involves verifying the patient’s insurance coverage and benefits to determine the amount of coverage the insurance provider will pay for medical services rendered. This process ensures that healthcare providers receive the correct reimbursement for services and that patients are aware of their financial responsibilities. Insurance benefit verification includes verifying the patient’s insurance eligibility, determining the patient’s copay or coinsurance, and obtaining authorization for services that require it. Accurate and timely insurance benefit verification can prevent claim denials and delays in payment, leading to improved cash flow for healthcare providers and increased patient satisfaction.
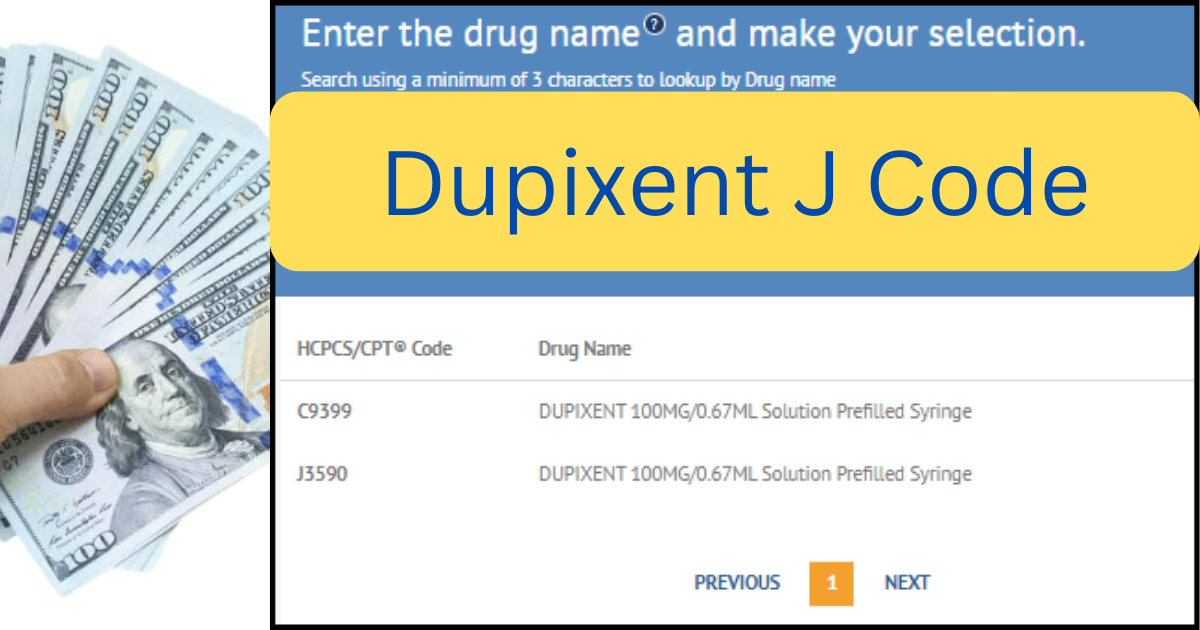
Medical coding:
Medical coding is another critical task in the RCM process. This involves assigning the correct medical codes to each patient encounter. Medical codes are used to describe the services provided to a patient and are used for billing purposes. An efficient coding process ensures that healthcare organizations are reimbursed accurately for the services they provide.
Medical Billing:
Billing is the next step in the RCM process. This involves submitting claims to the insurance provider for payment. A streamlined billing process helps to reduce administrative costs, increase revenue, and improve cash flow. Healthcare organizations can also use technology to automate the billing process, reducing the risk of errors and speeding up the payment cycle.
Claims submission:
Claims submission is another critical task in the RCM process. This involves submitting claims to the insurance provider for payment. An efficient claims submission process ensures that claims are submitted accurately and in a timely manner, reducing the risk of denials and rejections.
Posting Payment
Payment processing is the final step in the RCM process. This involves processing payments received from insurance providers and patients. An efficient payment processing system ensures that payments are processed accurately and in a timely manner, improving cash flow and reducing administrative costs.
By automating the payment posting process, healthcare organizations can reduce the risk of errors and speed up the payment cycle. Automation also frees up staff to focus on other critical tasks, such as denials management and patient care.
Data Analytics
Data analytics is a powerful tool that can help healthcare organizations to improve their RCM process. By analyzing data, healthcare organizations can identify areas of improvement, reduce denials, and increase revenue. Data analytics can also help healthcare organizations to identify trends and patterns that can be used to improve their operations.
For example, healthcare organizations can use data analytics to identify the most common denials and the reasons behind them. By addressing these denials, healthcare organizations can reduce the risk of future denials and increase revenue. Data analytics can also help healthcare organizations to identify areas where they can reduce costs, such as by reducing the number of claims that are denied or rejected.
Denial Management:
Now,
What is Denial Management?
Denial management is another critical component of the RCM process. Denials occur when insurance providers do not pay for a service that was provided to a patient. Denials can occur for various reasons, including incorrect coding, lack of documentation, or missing information.
By implementing an efficient denials management process, healthcare organizations can reduce the number of denials and increase revenue. Denials management involves identifying denials, appealing denials, and addressing the root cause of denials. Healthcare organizations can also use data analytics to identify the most common denials and the reasons behind them.
Conclusion
In conclusion, Revenue Cycle Management (RCM) is a critical financial process that enables healthcare organizations to track patient care services from the moment they are provided to the time they are paid. By implementing an efficient RCM process with data analytics, denials management, and payment posting, healthcare organizations can improve patient care, reduce costs, and enhance their financial performance. Data analytics can help healthcare organizations to identify areas of improvement, reduce denials, and increase revenue. Denials management can help to reduce the number of denials and increase revenue, while payment posting ensures that payments are processed accurately and in a timely manner. By investing in an effective RCM process, healthcare organizations can streamline their operations, reduce administrative costs, and increase revenue, resulting in better patient outcomes and a more prosperous business.