Medical coding is the process of assigning numerical or alphanumeric codes to medical diagnoses, procedures, and treatments for the purpose of billing and reimbursement from insurance companies or government programs. These codes are used to identify medical services and their associated costs, as well as to track and analyze healthcare data for research and quality improvement purposes.
Medical coding plays a crucial role in the healthcare industry, as it ensures that healthcare providers are properly reimbursed for their services and that insurance companies are charged accurately. It also facilitates the analysis and sharing of healthcare data, which is essential for improving patient outcomes and advancing medical research.
Responsibilities of a medical coder?
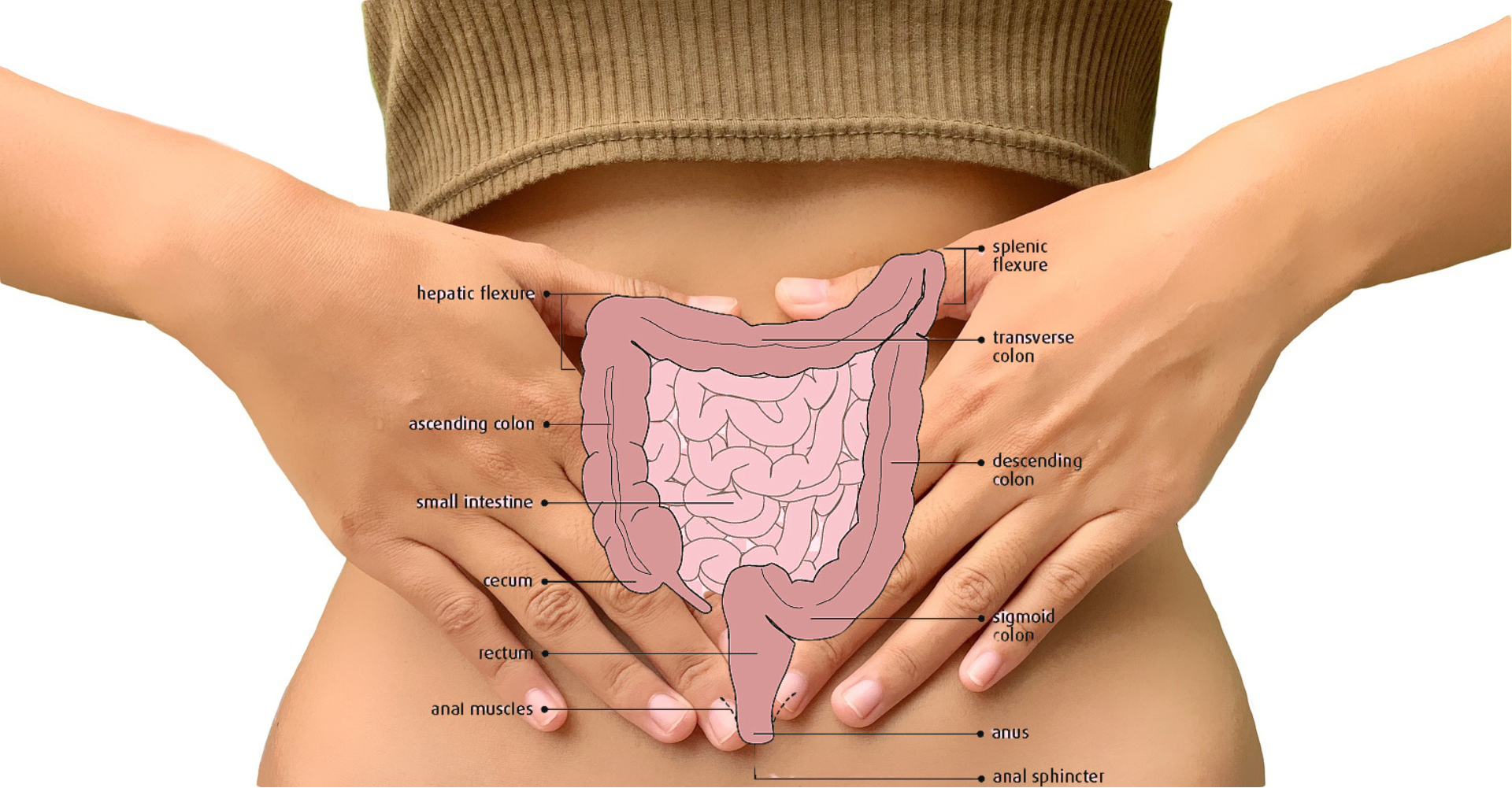
Medical coders are responsible for accurately translating the medical documentation provided by healthcare providers into these standardized codes. This requires a thorough understanding of medical terminology, anatomy, and physiology, as well as knowledge of coding guidelines and regulations.
As a medical coder, one of your main duties is to guarantee the precision of both the medical documents you transcribe and the codes you utilize. Along with this, you must also possess expertise in various medical codes and adhere to the code of ethics governing medical coding practices.
Your day-to-day responsibilities as a medical coder will typically include the following:
Converting patient information into the appropriate medical codes
Reviewing medical records and documents to identify any missing data
Conducting audits of patient charts
Gathering and organizing patient medical information
Ensuring that all documentation is grammatically correct
Adhering to medical coding guidelines and policies.
How to become a medical coder?
To become a medical coder, you need to follow these steps:
Meet the basic requirements:
To be eligible for medical coding training, you must have a high school diploma or a GED. You can complete medical coding training through an associate degree program in medical coding, a certificate program in medical coding from an accredited organization, or through on-the-job in-house training provided by your employer.
Complete medical coding training:
If you choose to pursue an associate degree in medical coding, you can enroll in a reputable program offered by a community college or vocational school. There are both in-person and online options available. Alternatively, if you prefer to earn a certificate in medical coding, consider gaining professional experience in the healthcare field you would like to work in, as many certificate programs require some prior experience in medical coding and/or an associate degree.
Obtain your medical coding certification:
You can obtain a medical coding certification after completing an associate degree in medical coding or without any degree at all. Entry-level certifications can help you secure a medical coding job, and you can pursue specialty medical coding certifications at any point in your career. A list of all medical coding certifications is available through the three major national accrediting organizations: PMI, AHIMA, or AAPC. Most certification programs include a final exam that you must pass to earn your certificate.
Brush up on your medical coding skills:
After completing training or obtaining your medical coding certification, it is crucial to refresh your skills and knowledge in the in-demand skills required for medical coding. You can enroll in a course on medical software or reimbursement models on platforms such as Coursera. You can also request additional training materials from your employer, specific to its needs as a healthcare provider.
Look for a job:
When you are ready to look for a job, consider what area of the healthcare industry you would like to work in and what qualifications you possess. For instance, if you are interested in pediatrics, you can focus your job search in that area. You can also apply for jobs in your area to gain professional experience or consider remote medical coding job opportunities.
How long does it take to become a medical coder?
The amount of time it takes to become a medical coder can vary depending on the individual’s level of education and training.
Typically, a medical coding certificate program can be completed in 6 to 12 months, while an associate degree program can take 2 years to complete.
In addition to formal education, individuals may also need to pass a certification exam to become a certified professional coder (CPC). The exam typically takes 4-5 hours to complete, and preparation for the exam can take several weeks or months depending on the individual’s level of experience and knowledge.
Overall, the time it takes to become a medical coder can range from a few months to several years, depending on the individual’s education and career goals.
Where do medical coders work?
Medical coders can work in a variety of settings, including physician’s offices, hospitals, clinics, government agencies, insurance companies, nursing homes, and assisted living facilities. They may also work remotely as freelancers or contractors.
Medical coding consultants can work for various healthcare offices and may travel or work remotely. They are responsible for checking the accuracy of medical records and may train other medical coders.
The federal government is a significant employer of medical coders, with opportunities available in federal agencies like the Army National Guard, US Air Force, and the Department of Veterans Affairs.
Hospitals and clinics are among the most common places of employment for medical coders. They typically have multiple billing departments that require many medical coders to ensure accurate medical billing.
Insurance companies may hire medical coders to review the accuracy and validity of medical claims submitted by healthcare providers. Medical coders working in these environments should have a high level of proficiency in medical coding.
Medical coders who work in nursing homes, assisted living facilities, hospice care centers, and other senior care facilities may work with medical codes that are specific to senior services.
Some medical coders work remotely, providing medical coding services as freelancers or contractors. However, remote medical coders must have proper training, reliable computer access, and an internet connection. Employers may also require remote coders to comply with HIPAA privacy and security requirements due to the nature of their work with medical records.
Conclusion:
In conclusion, medical coding is a crucial component of the healthcare industry, as it ensures proper billing and reimbursement for healthcare services, facilitates data analysis, and contributes to the advancement of medical research. Becoming a medical coder requires meeting basic educational requirements, completing medical coding training, obtaining certification, and keeping up with changes and developments in the field. Medical coders can work in a variety of settings, including hospitals, clinics, government agencies, insurance companies, and senior care facilities. The time it takes to become a medical coder varies based on education and career goals, and remote medical coding jobs are becoming increasingly popular. Overall, medical coding is an important and rewarding career path for those with an interest in the healthcare industry and a strong attention to detail.
Medical Coding FAQS:
What is medical coding?
Medical coding is the process of converting medical procedures, diagnoses, and symptoms into universal medical alphanumeric codes. These codes are used by healthcare providers to accurately and consistently document patients’ medical conditions and the services provided to them.
Why is medical coding important?
Medical coding is critical for accurate and efficient communication between healthcare providers, insurance companies, and government agencies. The codes allow for uniform documentation and billing, which helps to prevent errors, reduce costs, and improve patient care.
Who uses medical coding?
Medical coding is used by a variety of healthcare professionals, including doctors, nurses, medical billers and coders, insurance companies, and government agencies such as Medicare and Medicaid.
What are the different types of medical codes?
There are two main types of medical codes: Current Procedural Terminology (CPT) codes and International Classification of Diseases (ICD) codes. CPT codes are used to describe medical procedures, while ICD codes are used to describe medical diagnoses and symptoms.
How do medical coders ensure accuracy?
Medical coders must have a deep understanding of medical terminology, anatomy, and physiology, as well as a thorough knowledge of the coding system used. They typically receive extensive training and must pass a certification exam. Additionally, healthcare providers and coders work together to ensure that medical records are accurate and complete.